The Royal Thai Ministry of Public Health established the country’s National Malaria Program in the 1970s. Since then the program has identified a staggering 6 million cases of malaria. Starting in 2000, Thailand has stepped up its fight against malaria and aims to not only be the first country in the Greater Mekong Sub-region (GMS) to be malaria-free by 2024, but also receive the World Health Organization’s (WHO) certification as being malaria-free in 2027.
External funding has been instrumental in enabling Thailand to rollout free malaria screening and treatment services to communities in need, including targeting mobile, migrant, and other hard-to-reach communities. Universal coverage of indoor residual spraying (through domestic resources) and the distribution of insecticide-treated bed nets has been achieved in areas with high malaria transmission. Underpinning these efforts has been a commitment to strengthen the Malaria Information System and routine surveillance to better inform policy and programming. PMI support in Thailand has focused on strengthening the technical and programmatic capacity of the national malaria program. Together, these interventions helped to reduce the number of malaria cases from 203,394 in 1999-2000 to 35,825 in 2015-2016.
“We have the tools and technical capacity to eliminate malaria by 2024, what we’re lacking is sufficient funding. The cost-benefit analysis provides clear evidence for a high return of investment in the national malaria elimination strategy. The cost-benefit results conducted with support from USAID and Inform Asia has been used by the Country Coordinating Mechanism to develop [a] transitional plan and to advocate the funding gap. In previous years, our budget for [a] malaria control program average[d] around 3 to 4 million THB per year. In 2017, we received around 77 million THB to support funding gaps with a commitment to double the government funding in 2018.”
Dr Prayuth Sudathip
Center for Malaria Elimination Coordination
Bureau of Vector Borne Diseases,
Department of Disease Control
Ministry of Public Health, Thailand
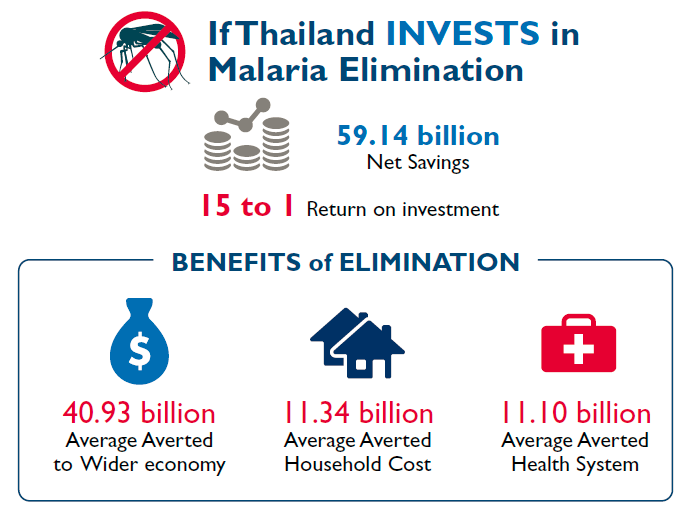
The CBA involved building a 20-year model for two scenarios: full investment in NMES and no investment in NMES. The key components of the model included projections of malaria cases and investment costs versus outcome costs (benefits) to quantify the return of investment for the NMES to achieve malaria-free status. The benefits were examined from the perspectives of the health system, direct cost to households, and the cost to the overall economy (i.e., downstream economic impact of a malaria case and tourism revenues). To ensure the validity of the model, inputs were obtained from decades of National Malaria Program data, as well as the national databases from the Ministries of Public Health, Interior, and Sports and Tourism. Other data were obtained from literature reviews and malaria experts from the World Bank, Asian Development Bank, and WHO. Finally, additional quantitative and qualitative data were gathered from key informant interviews to help support the CBA’s theoretical framework. Thailand’s national malaria technical working group was also consulted throughout the study to ensure that the CBA model was applied to the Thai context.
Key CBA findings: For every 1 Thai Baht (THB) invested in malaria elimination, a cost savings of 15 THB is expected.
In 2017, the National Malaria Program conveyed the CBA’s key message to multiple stakeholders in various forms, which resulted in the following achievements:
- The Prime Minister’s Office endorsed the NMES, thereby giving the strategy high-level political commitment. The Deputy Prime Minister of Thailand now chairs a national committee for malaria elimination.
- The Country Coordinating Mechanism (CCM) cited the CBA findings in the Global Fund transitional plan for 2018–2020.
- The CCM plans to replicate the CBA malaria elimination model for other disease control programs to communicate to decision makers for additional support and resources.
- The National Malaria Program successfully advocated that domestic funding be used to increase the national program budget to 77 million THB (20-fold increase) in 2017, with a commitment to double the increase in 2018. This is a significant contrast to 2016, when the domestic budget contribution to the National Malaria Program was around 4 million THB annually.
Beginning in 2018, the National Malaria Program, with support from PMI, plans to support subnational-level advocacy and operational planning. The increasing threat of multidrug resistant malaria in the GMS highlights Thailand’s need to stay vigilant in the fight against malaria. Armed with improved technical and programmatic capacity, political commitment, and increasing domestic resources, Thailand will be more self-reliant and better able to stay on course to achieve malaria elimination by 2024.