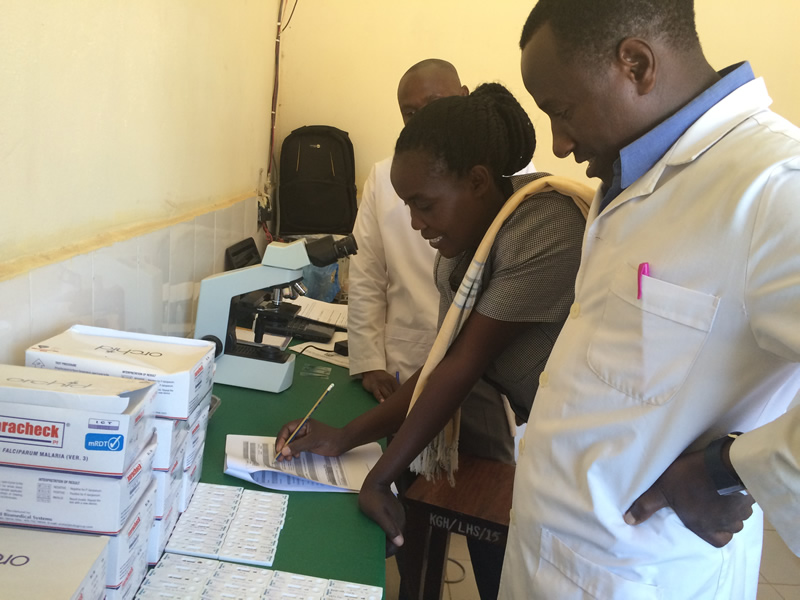
At a health facility in Tanzania, a supervisor provides feedback to staff after assessing performance. Photo credit: Dr. Goodluck Tesha, MalariaCare.
Currently, up to 40 percent of all people reported to have malaria in Tanzania have not received a confirmatory diagnostic test. Furthermore, the quality of testing performed by healthcare workers is often substandard. Recognizing the importance of accurate diagnosis, Tanzania is striving to ensure that all suspected malaria cases are tested using a rapid diagnostic test (RDT) or microscopy, and treated appropriately.
To this end, Tanzania’s National Malaria Control Program asked the President’s Malaria Initiative (PMI) to support a series of classroom training sessions for health workers followed by rounds of outreach training and supportive supervision by trained supervisors. The training and supervisory visits were conducted in five regions in Tanzania’s Lake Zone, an area with a very high incidence of malaria.
Initial training sessions emphasized proper use of RDTs to ensure accuracy and quality. Once the trainees returned to their health facilities, supportive supervision teams – a clinician and a laboratory expert – visited them onsite. The supervisory visits sought to build upon and reinforce the initial training, and to confirm the proper use of RDTs. The training and follow-up supervision involved more than 1,800 health care providers from 757 public health facilities.
Mr. Anthony Mlangwa, a clinician from a remote part of Simiyu region, attended one of the training sessions. He explained that before the PMI training, his normal practice was to clinically assess patients with fever and, in the vast majority of cases, automatically prescribe an antimalarial treatment. Even when he did use an RDT and the patient tested negative, he would typically prescribe quinine injections for fear that if he did not give an antimalarial to a child with fever, the child might die. He also felt that because patients often traveled long distances to see him, they should receive medication to take home. Sometimes patients even demanded antimalarials. His rationale for treating despite a confirmatory test was that the drugs would not do any harm, and might help.
Now, as a result of the PMI-supported training and supervision, Mr. Mlangwa has a much clearer understanding of appropriate malaria case management, including the importance of diagnosis followed by appropriate treatment. He makes sure that he has enough RDTs to meet demand, and he uses them with all febrile patients. He only gives antimalarials to those who test positive. In his remarks to the visiting supervisor, Mr. Mlangwa was proud to declare, “PMI support helps me save people’s lives. The training and supportive supervision increased my confidence in treating malaria. And I will strive to teach others that no patient should be given antimalarials before testing, and no patient should be given antimalarials if the result is negative.”
Though not all clinical and laboratory staff have the opportunity to attend training sessions, the supportive supervision received in clinics extends the number of health workers who benefit from the program. Mr. Kulwa Bahati, a nurse at a health dispensary in the Shinyanga region said, “I am not among those who was invited for skills training, but my colleagues who attended the sessions gave me feedback and on-the-job training after they returned. That was very good, but I confess that I still had some doubts, wondering if I had understood them well, or that maybe they forgot something. So when the supervisory team came to my clinic and included me in their observations, assessments, and RDT mentorship and feedback, I felt more empowered and confident in my knowledge and skills. The knowledge they shared helped me a lot. Now when I find myself alone at our facility, I am able to perform the RDT on my own and manage patients according to their test results.
“I promise that when they come for the next supportive supervision visit, our facility will score 100 percent on all the RDT testing accuracy indicators!” he exclaimed.
