A community mobilizer, tasked with alerting and sensitizing the community of the malaria campaign, poses with his megaphone. Photo credit: UNICEF
Fever, fatigue, head and muscle aches progressing to diarrhea and vomiting. Is it the flu? Possibly malaria? Or maybe Ebola? For the 447,000 people who live in the Beni Health Zone in the Democratic Republic of Congo (DRC), finding the answer and seeking appropriate care is a complex issue.
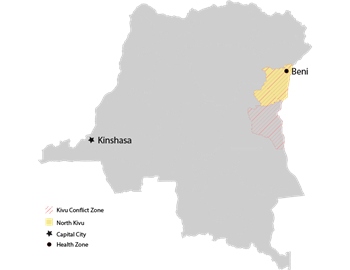
Beni Health Zone is in North Kivu, an area of DRC that has been rife with military conflict since the mid-2000s, and now the epicenter of the country’s largest ever Ebola outbreak—second only globally to the devastating West Africa outbreak of 2014–2016. The outbreak has caused 589 cases, of which 446 are confirmed including 283 deaths as of December 10 the DRC Ministry of Public Health reports.
Malaria, which mimics Ebola symptoms, also threatens the livelihood of the community. Although Malaria is both preventable and treatable, those who seek care at a health facility during an Ebola outbreak increase their exposure to the highly contagious Ebola virus. Yet untreated,malaria can also turn deadly, especially among young children and pregnant women.
Malaria burden on the rise
DRC is one of the highest malaria-burden countries in the world, following only Nigeria in estimated cases and deaths. But in North Kivu, which benefits from a generally high elevation that is unfavorable to malaria parasite-carrying mosquitos, less than five percent of the human population tested positive for the parasite during the most recent Demographic and Health Survey—low enough to qualify the area for malaria elimination activities.
However, just a few weeks after the Ebola outbreak was declared in August, malaria cases began to rise significantly, and by October the malaria outbreak warranted a response of its own.
A coordinated response
To achieve coverage of the vast, decentralized country, donors working in DRC such as the U.S. President’s Malaria Initiative (PMI) and the Global Fund have divided malaria programming by province. Though PMI does not normally work in North Kivu, when the call came in for support there was no hesitation.
Timeline
October 26: PMI asked to support malaria outbreak response in Beni Health Zone. PMI begins prepping to move nets.
October 28: Response plan shared with core malaria partners.
October 31: PMI determines channel to support operational costs.
November 2: First formal meeting of all partners supporting the malaria response takes place in Kinshasa.
Week of November 19: 250,000 bed nets transferred from Kinshasa and Bukavu to Beni.
November 27: All bed nets in place for distribution.
November 28: Campaign launch.
Within days, donors had shared a plan of action: a mass malaria drug administration and insecticide-treated bed net campaign targeting the entire health zone was to take place. PMI would provide 250,000 bed nets and cover associated operational costs through UNICEF; the WHO would provide training and supervision of community health volunteers plus child and adolescent malaria treatments; and the Global Fund would deliver 228,000 adult malaria treatments.
The approach was similar to one used during the West Africa outbreak, designed not only to treat malaria illness, but also relieve pressure on the overburdened health clinics.
By late November, the treatments and nets had made their way from Kinshasa to Beni and training was underway.
Reflecting on the donor coordination, Dr. Stefan Hoyer exclaimed, “In my experience of malaria control for WHO since 1991, I have never seen such enthusiasm and this level of high-quality, speedy, professional cooperation!”
But donor coordination isn’t enough, noted Marcos Patiño Mayer, the DRC malaria portfolio manager at the Global Fund. “Mass activities in such an insecure setting require a huge effort in communication and buy-in from the community.”
The campaign, which kicked off exactly a month after the National Malaria Control Program and local health authorities shared the first draft of the response plan with partners, organized over 4,500 local volunteers. Divided into teams of three people each, volunteers set out to reach 80,000 homes, providing malaria treatments and enough nets to cover each household entirely.
Volunteers were met with enthusiasm from the community, with residents in some locations coming out to the streets to ask for nets and drugs. After four days, the campaign concluded as planned on Saturday, December 1, having reached 88 percent.