In Senegal—which saw an estimated 836,000 malaria cases in 2020—effective treatment is critical.
“The only way to save patients’ lives is to make sure the drugs you administer are effective,” says Dr. Daouda Ndiaye of Senegal’s national parasitic disease laboratory. “In Senegal, this is crucial every day. Every hour.”
In 2015, Dr. Ndiaye and his colleague Dr. Awa Deme traveled to the Atlanta headquarters of the Centers for Disease Control and Prevention (CDC) to learn the latest methods in antimalarial resistance monitoring: DNA isolation, next-generation sequencing, bioinformatics, and photo-induced electron transfer PCR testing.
“I learned many new techniques which helped me feel confident with the results I was getting. This was very, very important to me,” remembers Dr. Deme. “I learned how labs should be organized which was something I implemented with my team back home.”
HOW MALARIA IS TREATED
Throughout much of the world, including Africa, health care providers typically treat malaria cases with a combination of drugs known as artemisinin-based combination therapy (ACT), the World Health Organization (WHO) recommended first-line treatment for uncomplicated malaria. These drugs—alongside the scale-up of other proven interventions such as insecticide treated bed nets, preventive medicines, and insecticide spraying, together with strengthened systems for malaria surveillance—are part of the reason the annual number of malaria deaths has been driven down significantly since 2000.
Fifteen years ago, malaria killed nearly 1.2 million people annually. Today, the collective efforts of USAID, CDC, and other global health partners have helped cut that number nearly in half.
However, continued long term drug efficacy should not be considered a foregone conclusion. Current antimalarial drug regimens cannot be relied upon forever. One of the looming threats to malaria elimination efforts around the world is the emergence and spread of parasites that are resistant to antimalarials like ACTs.
TESTING FOR DRUG REISTANCE IN AFRICA
To ensure ACTs are retaining their efficacy, CDC and PMI have been collaborating with African malaria researchers and national malaria control programs since 2015 to monitor drug resistance in Africa. We established the PMI-supported Antimalarial Resistance Monitoring in Africa (PARMA) network so malaria experts across Africa and the U.S. can work together to quickly identify emerging resistance and adapt treatment practices if necessary. For years, the WHO has supported countries to conduct drug efficacy trials. Streamlining and standardizing these efforts is one of PARMA’s primary objectives.
The work of the PARMA Network aligns with Goal 3.2 “Leverage investments in laboratory systems and field surveillance to strengthen global health security and mitigate against mosquito and parasite resistance” in the U.S. President’s Malaria Initiative Strategy 2021–2026 and Goal 2.4 “Advance laboratory methods to monitor and measure impact of malaria prevention, detection, control, and response efforts” in CDC’s Division of Parasitic Diseases and Malaria Strategies and Priorities 2021-2025
“Waning efficacy of drugs is an unfortunate eventuality for almost all pathogens we treat,” cautions Dr. Eric Halsey, a malaria researcher from CDC who supports PMI activities. “If you expose a pathogen to a drug long enough, it will eventually find a way to evade it. Just look at penicillin. For decades it was used to treat meningitis, pneumonia, gonorrhea, syphilis, and a dozen other infections. Today, penicillin is useful against syphilis and only a few other infectious diseases.”
Beginning in the late 1950s, parasites resistant to a different, widely-used antimalarial—chloroquine—emerged independently in Southeast Asia and South America. By the 1990s, parasite resistance to this drug stretched across the globe, including most of Africa. The problem was that nobody noticed initially.
Routine systems to monitor chloroquine effectiveness were simply not prioritized during that time and did not function very well. “Since the global community didn’t know how widespread the resistance was, there was a whole generation of children and adults being treated for malaria with an ineffective drug,” says Dr. Mateusz Plucinski, another researcher in CDC’s malaria branch. “That’s the worst-case scenario: something bad could be going on and nobody would know.”
Recently, PARMA collaborators identified artemisinin resistance in Rwanda. A few months later, artemisinin resistance was also identified in Uganda. ACTs are still working well throughout most of Africa, but these recent findings concern the global health community. If ACTs, the most widely used, well-tolerated, and cost-effective antimalarials in Africa, lose their effectiveness, it could set malaria control back by decades.
STRENGTHENING LABORATORY CAPABAILITIES IN AFRICA
CDC experts like Drs. Halsey and Plucinski have coordinated with their laboratory scientist colleagues at CDC—including Drs. Kumar Udhayakumar, Naomi Lucchi, and Eldin Talundzic—and African collaborators to test thousands of samples for ACT resistance in CDC’s Malaria Laboratory. “Usually, when we test samples, the efficacy of ACTs looks great,” reports Dr. Halsey. “However, this has started to change over the last three years. The PARMA network has made it more possible to uncover emerging resistance mutations.”
In addition to testing samples, experts from CDC’s Malaria Laboratory have also offered intensive eight-week trainings to African collaborators since 2015. As of April 2022, 15 African countries have sent laboratory experts to CDC’s Malaria Laboratory for training (including Drs. Awa Deme and Daouda Ndiaye).
“For me, the most important thing was seeing the great facility in Atlanta and getting to work with great people. They shared their experience and expertise with us and they continue to offer ongoing support,” says Dr. Ndiaye. “They really make sure we get the training and equipment we need, including the best techniques and using the latest technologies. CDC and PMI helped us with everything. We felt at home.”
COUNTRY-TO-COUNTRY SUPPORT
Continent-wide capacity for antimalarial resistance monitoring is vital since resistance spreads among parasites. As malaria-infected persons and mosquitoes travel and migrate, these drug resistant parasites can be distributed over broad geographic areas. Adding to the challenge, resistance can also independently emerge in an area.
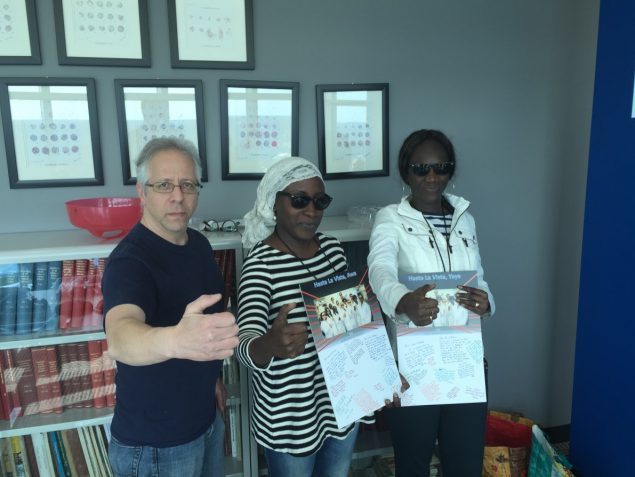
CDC Malaria Lab Manager Ira Goldman (left) poses with Senegalese malaria researchers Awa Deme (center) and Yaye Ndiaye (right) at the conclusion of their training at CDC Headquarters in Atlanta, GA.
The PARMA collaboration continues even after the trainees return home. CDC lab experts have traveled to Mali, Senegal, and Tanzania to offer additional laboratory support with the goal of having countries serve as regional PARMA training hubs, using what they’ve learned in the U.S. to train colleagues in neighboring countries.
“The work with collaborators in their home laboratories is just as important as the initial training. We want to ensure that trainees are supported to continue meeting their national malaria control programs’ needs,” says Dr. Meera Venkatesan, a PMI scientist working at USAID.
“It’s better for all this work to be done locally,” says Dr. Halsey. “My aspiration for PARMA is that more antimalarial monitoring work can be done in Africa so there’s less need to send samples to the U.S. or Europe for testing. That’s simply too expensive and slow.”
Dr. Ndiaye adds: “We are very lucky in Senegal. Our lab is one of the biggest and best in Africa. One of our goals now is to grow and train colleagues in other countries. We have the facility to train other countries’ scientists and we have the expertise; not just in malaria, but for other diseases, too.”
So far, Drs. Ndiaye and Deme, along with their teams, have provided support to researchers from Gabon, Benin, Ghana, Burkina Faso, Tanzania, and even some visiting American students.
This year, CDC Foundation and the Bill and Melinda Gates Foundation are supporting a PMI initiative to equip the lab at Cheikh Anta Diop University of Dakar, Senegal, so it can offer the same trainings and services available at CDC’s Malaria Lab.
Seeing the capacity to monitor for antimalarial resistance in Africa grow stronger demonstrates that PARMA is really working, says Dr. Halsey. “We welcome the growing decentralization. Sharing these responsibilities with our African collaborators is all part of the plan.”
“We want to help other countries feel that they can do this in their own countries,” says Dr. Deme. “The need for surveillance is urgent.”
