Malaria case management training includes the use of RDTs and ACTs, the recognition of danger signs, and referral of serious cases or any malaria in pregnant women or young infants to higher-level facilities.
Across Senegal, small one- or two-room huts in remote, rural areas, far from government health facilities, provide health care to local residents. Although not a part of the formal government system, Senegal’s health care pyramid rests on a foundation of almost 1,400 of these health huts. Local communities establish and manage the health huts, which provide services to nearly 20 percent of the country’s population.
Because malaria transmission is higher in rural areas, support to community-based care is critical to successful malaria control.
PMI and the USAID maternal and child health program have assisted these huts by offering training and a package of services. Although the services vary from village to village, most huts offer diagnosis and treatment of malaria and treatment for diarrhea, de-worming, growth monitoring and promotion, vitamin A supplementation, management of malnutrition, and family planning and reproductive health services. Literate community health workers can provide pneumonia case management with an antibiotic.
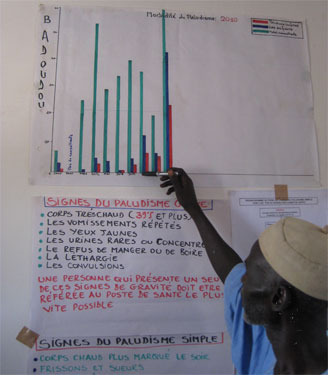
The president of the health committee in Badoudou, Senegal, shows the health data the committee has been tracking since the beginning of the year. Source: Caritas/Senegal
Malaria case management training includes the use of RDTs and ACTs, the recognition of danger signs, and referral of serious cases or any malaria in pregnant women or young infants to higher-level facilities.
Overall, community health workers at health huts in Senegal have demonstrated excellent adherence to the treatment protocol and malaria rates have plummeted. Not only is better case management reducing the number of unnecessary treatments, which are expensive, but it also allows community health workers to focus on the other illnesses that were previously confused with malaria.

