Using Senegal’s existing PECADOM (Prise en charge à domicile) model, volunteer health care workers were trained on home-based management of malaria and paid a small wage (approximately $5 per week) to conduct weekly door-to-door visits in their village to detect and treat all suspected malaria cases.
Peace Corps volunteers are partnering with Senegal’s NMCP and PMI to study a new approach to malaria testing and treatment for rural populations with limited access to health care. The aim of the project is to actively detect and treat all malaria cases, thus diminishing the reservoir of malaria parasites in humans. The approach is to train health workers and residents on active surveillance, testing, and treatment. Using Senegal’s existing PECADOM (Prise en charge à domicile) model, volunteer health care workers were trained on home-based management of malaria and paid a small wage (approximately $5 per week) to conduct weekly door-to-door visits in their village to detect and treat all suspected malaria cases. One woman from each household was also trained to recognize symptoms to assist health workers to locate possible malaria cases, ensuring everyone in the village was monitored for malaria and all symptomatic people received free testing and treatment.
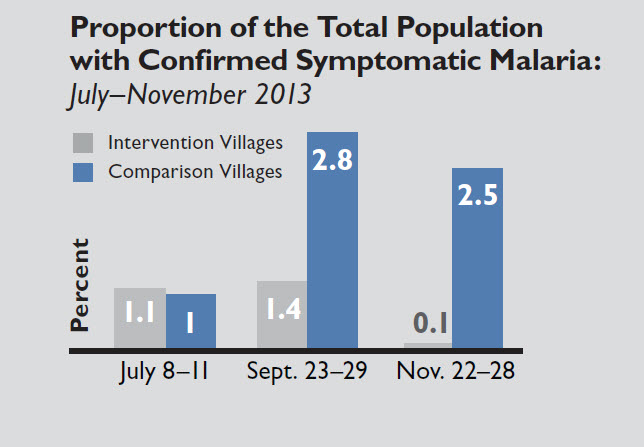
After a promising pilot conducted in one village during 2012, this model was expanded to 15 villages in the Saraya Health District during the 2013 malaria transmission season (July–November). Fifteen comparison villages were chosen among villages benefiting from the original passive PECADOM model. Active case detection surveys were conducted in both the intervention and comparison villages to estimate symptomatic malaria prevalence at baseline, midline, and endline. At baseline, both sets of villages showed a similar prevalence at just around 1 percent. In the end, the prevalence in comparison villages was much higher than in the intervention villages, where only 6 cases of symptomatic malaria were found, showing great promise for this model.