In 2008, a President’s Malaria Initiative (PMI)-supported indoor residual spraying (IRS) program was instituted in five districts in the Northern Region of Ghana. This region is an important focus for the Government of Ghana because it has higher rates of malaria transmission, less access to health care resources, and lower economic development, compared to other regions of the country. Northern Ghana has a tropical savannah climate with one major transmission season, August to November, during which the majority of cases occur. In 2011, IRS was implemented in Bunkpurugu Yunyoo District, Northern Region, using a pyrethroid insecticide (alpha-cypermethrin – Fendona®, BASF, Ludwigshaften, Germany). In 2013, the insecticide was changed to a long-lasting organophosphate (pirimiphos-methyl – Actellic CS®, Syngenta, Basel, Switzerland) due to pyrethroid resistance. Spraying was conducted April–June, prior to the rainy season and the subsequent high malaria transmission season. Previous monitoring studies in the Northern Region revealed that pyrethroids and organophosphates last at least 6 months (> 80 percent mortality of susceptible mosquitoes) and, therefore, could be expected to provide adequate coverage during the entire transmission season. Mass distributions in Bunkpurugu Yunyoo District of long-lasting insecticide (pyrethroid)-treated mosquito nets were conducted in August 2010 and August 2012.
Childhood Anemia and Parasitemia Surveys and Entomological Monitoring in Bunkpurugu Yunyoo District
Between 2010 and 2013, cross-sectional anemia and parasitemia surveys were conducted in Bunkpurugu Yunyoo District to assess the impact of malaria control efforts, primarily IRS. This impact was assessed by the prevalence of anemia and asexual malaria parasitemia, as determined by blood hemoglobin levels (g/dl) using Hemocue and microscopy, in children under five during the high malaria transmission season, August–November. Sampling of communities within Bunkpurugu Yunyoo District was proportional to size, compounds within the community were randomly sampled, and all children under five in the chosen compound recruited for testing. Informed consent was sought from caregivers. The study included a questionnaire, which covered family demographic and socio-economic characteristics, nutrition, access to malaria care, malaria interventions (i.e., IRS, mass distribution of insecticide-treated mosquito nets, and malaria prophylaxis among pregnant women), and child-specific questions about illnesses, hospitalizations, and medications, asked of the primary caregiver. The survey also included the administration of a malaria rapid diagnostic test (RDT), with administration of appropriate malaria treatment to those who tested positive and had a recent history of fever (48 hours prior to survey, as measured or reported), in accordance with Ghana’s malaria treatment guidelines. Children with other illnesses were provided appropriate referrals based on signs and symptoms of illness, or were transported to the area’s primary referral hospital if they exhibited symptoms of serious illness.
PMI has conducted entomological monitoring in four districts in the Northern Region, including Bunkpurugu Yunyoo District during the anemia and parasitemia study period, 2010–2013. Indoor resting densities (IRD), parity, sporozoite rate and entomological inoculation rates (EIR) of the local vector species have been monitored annually since 2010 via monthly human landing and pyrethrum spray collections. EIR is the product of the mosquito population’s plasmodium infection rate and the mosquito’s biting rate and is expressed below as a nightly EIR.
Results of Anemia and Parasitemia Survey during Use of Pyrethroids, 2010–2012
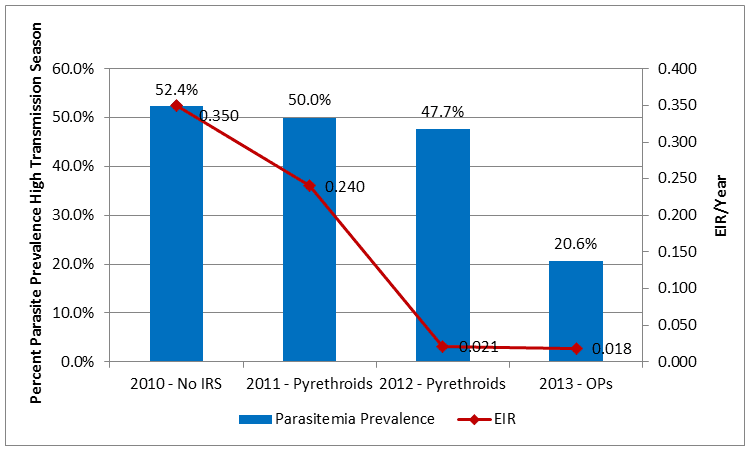
IRS was not implemented until 2011, thus 2010 served as the pre-IRS baseline. During the period of pyrethroid use, anemia had a statistically significant decrease, from 77.7 percent to 67.8 percent (p<0.001) between 2010 and 2012 among children under five in Bunkpurugu Yunyoo District, while the decline in parasitemia was more modest, but still statistically significant, from 52.4 percent to 47.7 percent (p=0.005) (Table 1 and Figure 1). The percent of children with an RDT-positive result also showed a statistically significant, but not dramatic decrease, 69.9 percent to 66.0 percent (p=0.01). However, the percent of children with fevers had a statistically greater decrease, from 69.4 percent to 43.9 percent (p<0.001). Insecticide-treated mosquito net use was approximately 95 percent in 2010, but dipped to 82.2 percent in 2011 and increased to 93.6 percent in 2012. During pyrethroid use, the EIR showed a dramatic, statistically significant decline from 0.350 infective bites/person/night in 2010 to 0.021 in 2012 (p=0.018) (Figure 1).
Results of Anemia and Parasitemia Survey after Organophosphate Introduction, 2013
After the switch to organophosphates in 2013, the prevalence of anemia and parasitemia in children under five showed a large and statistically significant decrease, from 67.8 percent to 48.3 percent (p<0.0002) and 47.7 percent to 20.6 percent (p<0.001) respectively, between 2012 and 2013 (Table 1). The other health indicators also showed large and statistically significant decreases between 2012 and 2013: Percent RDT-positive from 66.0 percent to 29.2 percent (p<0.0002) and percent with fever from 43.9 percent to 22.1 percent (p<0.0002) (Table 1). There was also a statistically significant decrease in the use of insecticide-treated mosquito nets on the night preceding the survey, from 93.6 percent to 68.5 percent (p<0.0002), even though a mass distribution campaign was conducted in 2012. The EIR in 2013 remained statistically unchanged at 0.018 infective bites/person/night compared to 0.021 in 2012 (p=0.1031) even after the switch to the organophosphate (pirimiphos-methyl CS).
Discussion
The impact of malaria control activities, including IRS using pyrethroids, was not large when anemia and parasitemia rates were measured, but statistically significant drops in mosquito transmission were estimated when EIRs were calculated. In contrast, there was a large decrease in anemia and parasitemia after the switch to the organophosphate, yet no further reduction in EIR after the switch in 2013. Although the pyrethroid used did not appear to have an impact on anemia and parasitemia rates as dramatically as did the organophosphate, it seems clear that the long-term use of an effective insecticide reduced anemia and parasitemia prevalence in children under five as well as EIRs in Anopheles vector populations. It remains unclear however, why a lag in anemia and parasitemia reduction occurred (in 2013) when the EIR was already greatly reduced in 2012. In examining the impact of IRS, this preliminary analysis does not fully take into account the level and intensity of all the different malaria control strategies employed in Bunkpurugu Yunyoo District during the study period. We hope that the 2014 anemia and parasitemia survey and ongoing entomological monitoring will provide other important, as well as longitudinal, information to maximize the impact of IRS.
Table 1: Selected Indicators from Anemia & Malaria Parasitemia Surveys, Children Under five, Bunkpurugu Yunyoo, 2010–2013 High Transmission Seasons
| 2010 November No IRS (N=1,923) |
2011 October Pyrethroids (N=2,040) |
2012 October Pyrethroids (N=2,026) |
2013 November Organophosphates (N=1,311) |
|
| Percent with asexual malaria parasitemia
(95% C.I.) |
52.4%
(50.0 – 54.8) |
50.1%
(47.9 – 52.3) |
47.7%
(45.5 – 49.9) |
20.6%
(18.4 – 22.9) |
| Percent with RDT-positive result
(95% C.I.) |
69.9%
(67.9 – 72.0) |
70.4%
(68.4 – 72.4) |
66.0%
(63.9 – 68.1) |
29.2%
(26.8 – 31.8) |
| Percent with fever, recorded or reported past 48 hrs
(95% C.I.) |
69.4%
(67.3 – 71.5) |
59.0%
(56.8 – 61.1) |
43.9%
(41.7 – 46.1) |
22.1%
(19.9 – 24.5) |
| Percent with anemia (Hb<11g/dl)
(95% C.I.) |
77.7%
(75.8 – 79.5) |
72.5%
(70.5 – 74.4) |
67.8%
(65.7 – 69.9) |
48.3%
(45.6 – 51.0) |
| Percent sleeping under net, previous night
(95% C.I.) |
95.0%
(93.9 – 95.9) |
82.2%
(80.5 – 83.8) |
93.6%
(92.5 – 94.6) |
68.5%
(65.9 – 71.0) |
Figure 1: Malaria Parasitemia Prevalence in Children under Five during High Transmission Season and District Nightly Entomological Inoculation Rate (EIR), Bunkpurugu Yunyoo District, 2010–2013