In 2012, AIRS partnered with the government to pilot the model of using health extension workers to implement community-based indoor residual spraying (IRS).

Tigist Legesse, a health extension worker in Kersa district in Ethiopia, meets with a family to prepare their house for IRS. Credit: Yemane Yihdego, AIRS Ethiopia.
By training existing cadres of health extension workers in Ethiopia to lead indoor residual spraying (IRS)—an intervention that protects millions of people from malaria—the Africa Indoor Residual Spraying project (AIRS) was able to carry out IRS better, faster, and cheaper.
In Ethiopia, approximately 85 percent of the population lives in rural areas. To increase the rural population’s access to basic health services, the government of Ethiopia trained more than 30,000 health extension workers, mostly women, and deployed them to more than 15,000 village-based health posts.
In 2012, AIRS partnered with the government to pilot the model of using health extension workers to implement community-based indoor residual spraying (IRS). Traditionally, IRS is organized by the district health office, including selection, training, and deployment of spray operators.
AIRS trained health extension workers on 1) spraying and training techniques; 2) supervision and data recording; 3) spray pump maintenance; 4) environmental compliance and human safety; and 5) information, education, and communication. Using their new knowledge, health extension workers recruited and trained spray operators and planned and implemented IRS in their villages.
AIRS observed the following results when carrying out the IRS campaign at the community-level as opposed to the district-level:
-
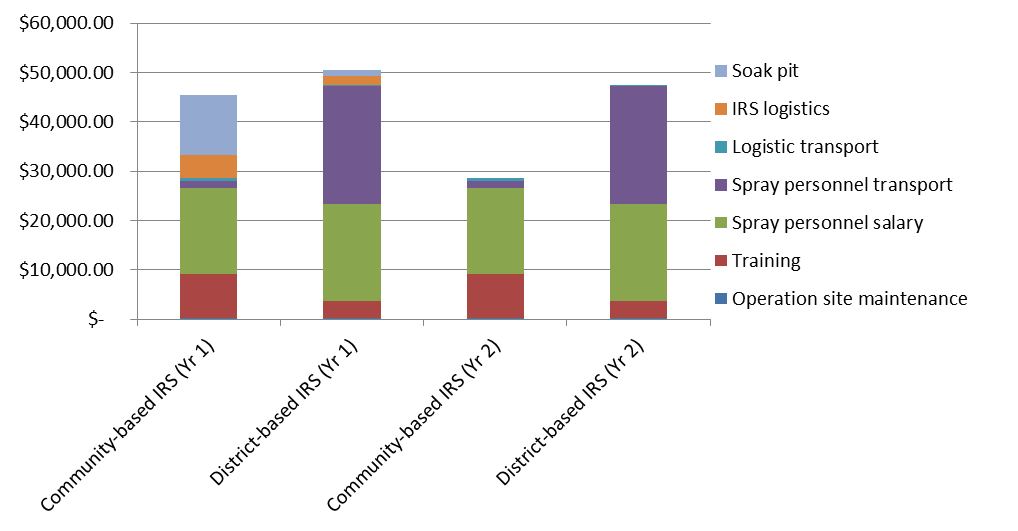
- Cost-effective. AIRS estimates that community-based IRS cost approximately 10 percent less than district-based IRS during the 2012 campaign and is anticipated to cost 40 percent less during the August 2013 campaign. Since operational sites were within walking distance of spray operators’ homes, providing camping at the site and renting vehicles to transport spray operators (one of the greatest expenses of spray operations) was not necessary. (See graph)
Preliminary Cost Analysis of Community-based IRS and District-based IRS
- Fast. More spray operators were hired, which means the campaign took fewer days to complete. Since spray operators live in the community, it is easy to mobilize them in case of an unexpected malaria outbreak or longer than usual transmission period.
- High quality. As a result of the low trainer-spray operator ratio of 2:5, spray operator received personal attention during trainings led by health extension workers. Recruiting spray operators from the village where they live resulted in strong feelings of ownership, close supervision by village leaders, and higher acceptance of IRS by the community. Additionally, theft and misuse of insecticide was less likely.
As a result of the successful community-based IRS pilot, the President’s Malaria Initiative (PMI), which funds AIRS, asked AIRS to expand the program to six additional districts in 2013. Similarly, the government of Ethiopia is preparing to replicate the community-based IRS model in all the IRS regions it directly manages. The Ministry of Health asked AIRS to prepare a training manual and implementation guidelines that can be used to as a reference by the health extension workers to scale up implementation community-based IRS throughout the country.
This story was taken from www.africairs.net
